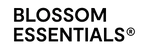
A potent blend of organic Manuka honey, nourishing oils, and natural moisturizers penetrates deeply to intensely hydrate, relieve dryness, and repair the skin barrier. This salve quickly soothes damaged, itchy skin, leaving it rejuvenated, healthy, and wonderfully soft.
Navigating Common Skin Concerns
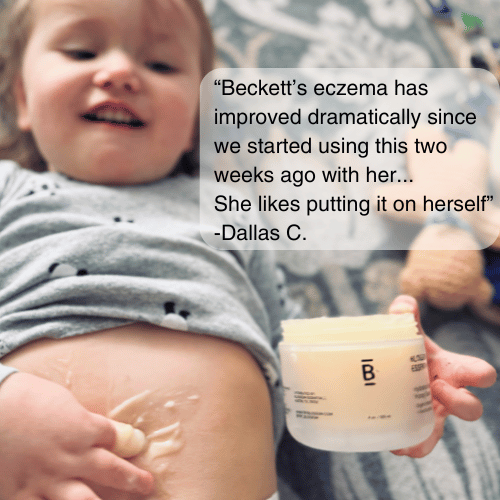
MANAGING PSORIASIS
Living with psoriasis? We get it. It's more than just a skin condition – it's a journey. As part of Blossom’s Navigating Skin Concerns series, we're diving deep into psoriasis, offering you a blend of scientific insights and practical tips. From causes to treatments, we've got you covered. Ready to take back control of your skin health? Let's get started!
THE PSORIASIS LOWDOWN
Psoriasis is a chronic autoimmune condition that affects millions of people worldwide. This persistent skin disorder disrupts the body's natural cell turnover process, causing skin cells to multiply much faster than usual. In areas affected by psoriasis, the skin cell lifecycle is dramatically shortened from the typical month-long cycle to just a few days. This rapid turnover results in the characteristic patches of thick, red, and scaly skin that can appear anywhere on the body, from the scalp to the feet.
Now, we need to understand that psoriasis is more than just a surface-level skin condition. It involves a complex interplay of genetic factors, immune system irregularities, and environmental triggers. Psoriasis manifests in several forms, with plaque psoriasis being the most common. Other types include guttate, inverse, and pustular psoriasis, each with its unique characteristics. While dealing with psoriasis can be challenging, it's worth noting that many people, including some public figures, have openly shared their experiences with the condition, and while we might not be able to cure it, there are plenty of things we can do to help reduce the symptoms and make living with psoriasis much easier!

PSORIASIS CAUSES AND SYMPTOMS
The exact cause of psoriasis remains a bit of a mystery, but over the years, researchers have identified several key factors that play a role in its development. At its core, psoriasis is an autoimmune condition where the body's defense system goes a little haywire. T-cells, typically our skin's protectors, mistakenly attack healthy skin cells, triggering inflammation and accelerated skin cell growth. This immune system mix-up is believed to have a genetic component, with certain genes increasing the likelihood of developing psoriasis. However, having these genes doesn't guarantee you'll develop the condition - environmental factors often act as the spark that ignites the psoriasis flame.
Speaking of sparks, let's talk about triggers. These are the external factors that can cause a psoriasis flare-up or worsen existing symptoms. Common culprits include stress, skin injuries (even a simple scratch can trigger a flare, known as the Koebner phenomenon), certain medications, and infections. Some people find that cold weather turns their skin into a psoriasis playground, while others notice flare-ups after soaking up too much sun. And for those who enjoy a glass of wine or a puff on a cigarette - sorry to be party poopers, but both alcohol and smoking have also been linked to increased psoriasis severity.
Now, onto the symptoms. Psoriasis is like a chameleon, presenting differently from person to person, but there are some classic signs to watch out for. The hallmark of psoriasis is patches of thick, red skin covered with silvery scales. These patches, known as plaques, can appear anywhere on the body but are most common on the knees, elbows, lower back, and scalp. They might be a little itchy, or they might feel like your skin is almost burning up. Some people experience nail changes, with pits, ridges, or thickening of the nails. In more severe cases, psoriasis can affect the joints, leading to psoriatic arthritis. Remember, psoriasis is more than skin deep - it can also come with fatigue, and the emotional impact of living with a visible skin condition shouldn't be underestimated. But don't worry, we're here to help you navigate all aspects of this condition!

PSORIASIS SOLUTIONS
While there's no cure for psoriasis, various treatments can help manage symptoms and improve quality of life. It's important to work with a healthcare provider to find the right combination of treatments for your specific case and never try to self-medicate. In this section, we'll take a quick look at some different approaches to managing psoriasis, from prescription medications to over-the-counter products and even a few natural remedies.
1. PRESCRIPTION MEDICATIONS
Prescription treatments are often necessary for moderate to severe psoriasis. These medications work to reduce inflammation, slow skin cell growth, or modulate the immune system. Always consult with a dermatologist before starting any prescription treatment. Prescriptions might include:
- Topical corticosteroids: These reduce inflammation and relieve itching. Use as directed to avoid skin thinning.
- Vitamin D analogues: Synthetic forms of vitamin D that slow skin cell growth. They're often combined with corticosteroids.
- Retinoids: Derivatives of vitamin A that can help with skin cell turnover. They may increase sun sensitivity.
- Biologics: Injectable medications that target specific parts of the immune system. Effective for moderate to severe cases.
- Methotrexate: An oral medication that suppresses the immune system and slows skin cell growth.
2. OVER-THE-COUNTER PRODUCTS
For milder cases or as complementary treatments, over-the-counter products can be helpful in managing psoriasis symptoms.
- Salicylic acid: Helps remove scales and reduce swelling. Available in various forms like shampoos and ointments.
- Coal tar: It’s been used in the battle against psoriasis for decades, and can slow skin cell growth and reduce inflammation. Often found in shampoos, creams, and bath solutions.
- Moisturizers: Essential for reducing dryness and itching. Look for fragrance-free, hypoallergenic options.
- Hydrocortisone creams: Mild steroids that can temporarily relieve itching and inflammation.
- Scale lifters: Products containing ingredients like urea or lactic acid can help remove scales.
3. NATURAL REMEDIES
While not a substitute for medical treatment, some natural remedies may help alleviate psoriasis symptoms when used in conjunction with other treatments.
- Aloe vera: One of nature’s top moisturizers, aloe may help reduce the redness and scaling that comes with psoriasis. Look for creams with 0.5% aloe content.
- Dead Sea salts: Adding these to a warm bath may help remove scales and ease itching.
- Oatmeal baths: Can provide temporary relief from itching and dryness.
- Tea tree oil: Some find it helpful for scalp psoriasis when used in shampoos.
- Turmeric: Its anti-inflammatory properties may help reduce psoriasis flares when taken as a supplement.
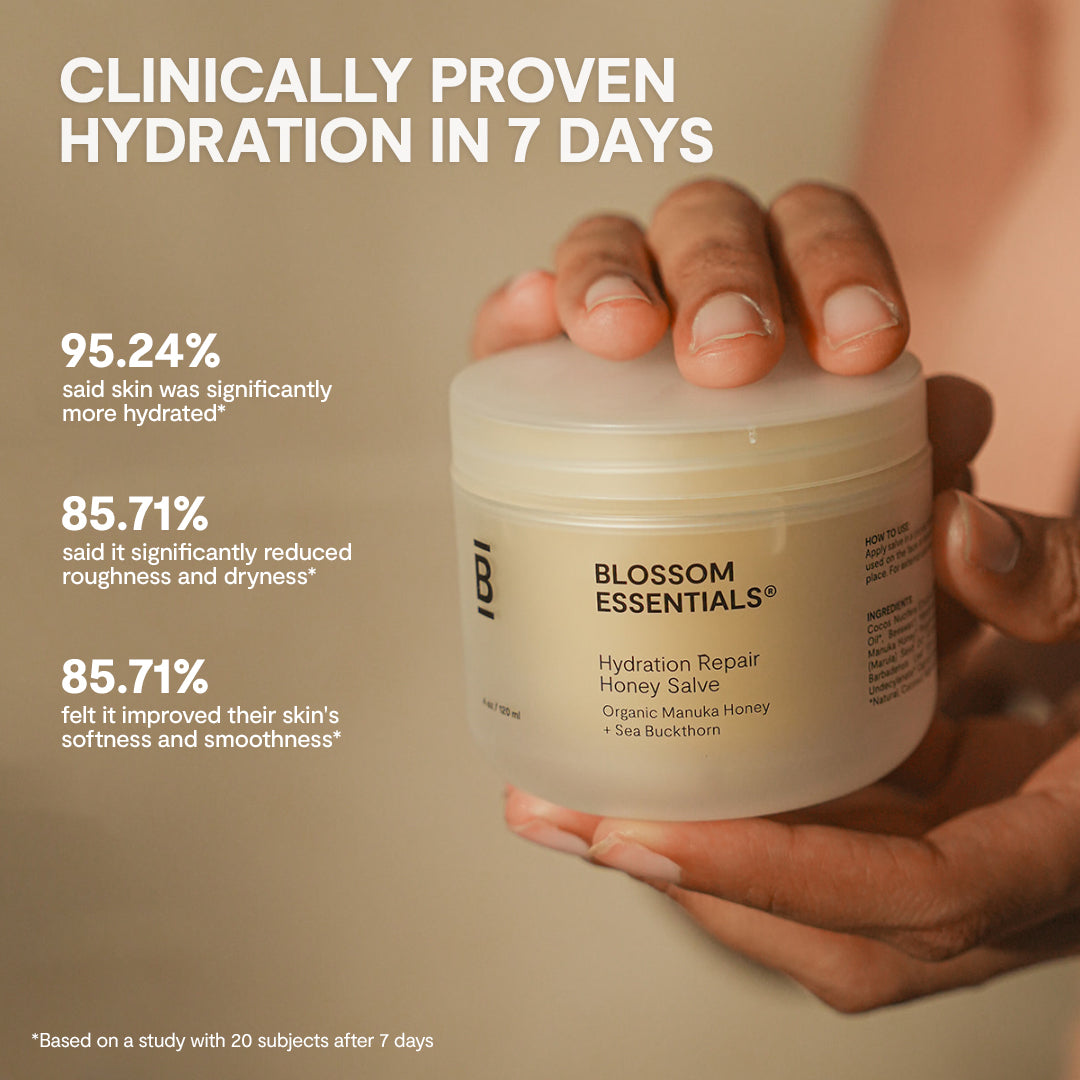
At Blossom, we understand the challenges of managing psoriasis. While we don't claim to cure the condition, our products are formulated with ingredients that may help soothe and hydrate psoriasis-prone skin. Our soothing Total Moisture Body Wash contains aloe vera, known for its potential to reduce redness and scaling. Additionally, our Hydration Repair Honey Salve is enriched with natural oils that can help keep skin moisturized, which is crucial for managing psoriasis symptoms.
Remember, what works for one person may not work for another. It's essential to consult with a healthcare provider before starting any new treatment regimen, especially when combining different approaches.

PSORIASIS-FRIENDLY SKINCARE ROUTINE
Living with psoriasis doesn't mean you can't enjoy a pampering skincare routine. In fact, a consistent regimen can help manage symptoms and keep your skin feeling its best. The key is to use gentle, nourishing products that won't irritate your skin or trigger flare-ups. At Blossom, we've crafted a range of products that can help alleviate the symptoms of sensitive, psoriasis-prone skin. Let's walk through a daily routine that combines effective care with a touch of self-love.
MORNING
- Cleanse: Kick off the routine with a gentle application of our Hydration Boost Face Cleanser. It’ll wash away dirt that has built up over night and boost your skin’s morning moisture levels.
- Moisturize: We’d recommend our Manuka Honey Salve for the face and Moisture Restore Lotion for the body. Both are full of naturally sourced oils and other ingredients that will help keep your skin hydrated.
- Protect: Don’t forget your sun protection! It won’t cure your psoriasis, but cancelling out those damaging UV rays can help prevent more unnecessary damage to your skin.
DAYTIME
- Soothe: If you experience itching or discomfort throughout the day, a soothing aloe vera gel could help provide quick, temporary relief.
EVENING
- Cleanse: Gently remove any makeup and contaminants that have built up during the day with our Hydration Boost Face Cleanser.
- Moisturize and Recover: Prep your skin for the night to come with our rich Hydration Recovery Face Cream.
BONUS PSORIASIS-SOOTHING TIPS
- Stay hydrated by drinking plenty of water throughout the day.
- Manage stress through relaxation techniques or gentle exercise.
- Use a humidifier in dry environments to add moisture to the air.
- Avoid hot showers and opt for lukewarm water instead.
- Pat your skin dry gently after bathing, and apply moisturizer immediately.
Remember, consistency is key when it comes to skincare routines. While these products can help manage symptoms, they're not a cure for psoriasis. Always consult with your dermatologist about incorporating new products into your routine, especially during flare-ups.
Psoriasis Mythbusting
Ridiculous! Psoriasis is an autoimmune condition and cannot be spread through physical contact.
While it can cause dry, flaky patches, psoriasis is a complex autoimmune condition affecting skin cell production.
Psoriasis can also impact joints (psoriatic arthritis) and increase the risk of other health conditions.
While regulated UV light exposure can help some cases, tanning beds are unsafe and can even worsen symptoms long-term.
It varies, but some foods may indeed trigger inflammation, while others might help manage symptoms. Diet can play a role in psoriasis management, so consult with your dermatologist.
While psoriasis can go into remission, it's a chronic condition that typically requires ongoing management.

LIVING WITH PSORIASIS
Psoriasis is more than just a skin condition - it's a journey that can affect various aspects of your life. But here's the good news: with the right mindset and strategies, you can lead a fulfilling, happy life while managing your psoriasis. Let's explore some ways to embrace your skin and thrive:
- Find Your Psoriasis Care Dream Team: Build a support network of healthcare professionals you trust. This might include a dermatologist, a therapist, and perhaps a nutritionist. Regular check-ups and open communication with your team can help you stay on top of your condition.
- Stress Less, Live More: Stress can be a major trigger for psoriasis flares. Explore stress-management techniques that work for you - whether it's meditation, yoga, deep breathing exercises, or a relaxing hobby. Remember, taking time for self-care isn't selfish; it's necessary.
- Nourish Your Body: While there's no one-size-fits-all diet for psoriasis, many people find that certain foods can help or hinder their symptoms. Consider keeping a food diary to identify your triggers. Generally, a balanced diet rich in anti-inflammatory foods like fruits, vegetables, and omega-3 fatty acids can support overall skin health.
- Move Your Body: Regular exercise can help manage stress, maintain a healthy weight, and potentially reduce inflammation. Find activities you enjoy - whether it's swimming, cycling, or dancing in your living room. Listen to your body and choose exercises that don't irritate your skin.
- Dress for Comfort and Confidence: Choose clothes that make you feel good and don't irritate your skin. Soft, breathable fabrics like cotton can be more comfortable during flare-ups. Don't let psoriasis dictate your style - find ways to express yourself that align with your skin's needs.
- Be Open About Your Needs: Whether at work, in relationships, or social situations, don't be afraid to communicate your needs. If you need to take breaks to apply moisturizer or avoid certain activities during flare-ups, that's okay. Your well-being comes first.
Living well with psoriasis is about finding what works for you. It's okay to have tough days, but don't let them overshadow the beautiful, unique individual you are. Your skin is just one part of your story - and you're the author of that story. Write it with love, care, and a touch of Blossom's nurturing spirit.

Frequently Asked Questions
Psoriasis can affect anyone, but studies suggest it's more prevalent in Caucasians and less common in people of African or Asian descent. However, when it does occur in people with darker skin, it can be more difficult to diagnose.
It can, but it doesn't have to! Open communication about your condition can help build trust. Remember, confidence is attractive, and your psoriasis doesn't define you. Many people with psoriasis have fulfilling relationships.
Yes, it can. Some people with psoriasis develop uveitis, an inflammation of the eye that can cause pain, redness, and vision problems. Regular eye check-ups are important if you have psoriasis.
Research has shown that people with severe psoriasis may have a slightly higher risk of cardiovascular issues. This is thought to be due to the systemic inflammation associated with psoriasis. Regular check-ups with your doctor can help monitor your overall health.
While psoriasis primarily affects the skin, some forms can impact internal areas. For example, erythrodermic psoriasis can affect large areas of the body, including mucous membranes. Always consult a healthcare provider about unusual symptoms.
It certainly can! Up to 50% of people with psoriasis experience nail changes. This can include pitting, discoloration, and separation of the nail from the nail bed. Keeping nails short and using gentle nail care products can help manage these symptoms.
Yes, psoriasis can develop at any age, including in children. In fact, about one-third of psoriasis cases begin in childhood. The symptoms and treatments may differ slightly for children, so pediatric dermatologist care is important.
Some studies suggest a potential link between psoriasis and celiac disease, with both involving immune system dysfunction. If you have psoriasis and experience digestive issues, it's worth discussing with your doctor to explore any potential connections.